Can the LV ejection fraction change with every heart beat ?
EF % is one of the glamorous cardiac functional indices that has caught the imagination of both patients and physicians. How accurate it is ? How reproducible it is ? How many methods are available to arrive at EF % ?
How many of us realise it can potentially change with every heart beat ? *
Apart from the heart rate dependency , the echocardiographic error can be amplified by
- Difficulty in identifying the leading and trialling edges of endocardium
- Patient posture errors
- Edge detection errors in 2D
- Pap muscle shadowing .
- Angle errors
- Sub optimal echo windows when EF is measured in the bed side in critical care units
- Mental status of performing sonographer/cardiologist (One who chops 2D shells hurriedly and obliquely ! )
All these make this index a highly variable parameter( next only to your city temperature ! ) This happens whether you measure EF with M Mode, 2D Simpson , 3D volumetric etc .
* The term “beat to beat” changes may be a little exaggerated statement .It is used to convey the point of ” huge variability” of this parameter. It means there can be variations of EF % with varying heat rate.
The heart is not an Independent organ rather, it is a slave to preload and afterload !
How to overcome the limitation of EF ?
To overcome this error a new parameter called myocardial performance index (MPI) which accounts for heart rate came into vogue . (Did it come really ? Ihaven’t seen a single cardiologist do this in his clinic ) . 3D volumetrics, velocity vector imaging , and many other innovations has been added. Nothing was able to replace the EF % . Because of complexities in the newer modalities most cardiologists (including the author ) continue to romance the much flawed EF % .
Simplicity shall reign supreme . . . in spite of inaccuracies , in any walk of life !
How does EF change beat to beat ?
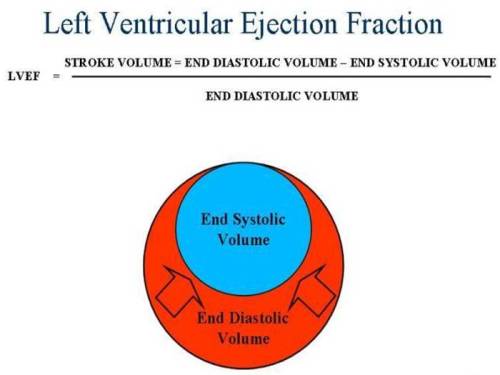
The answer is simple . The contractility of heart is dependent upon the previous diastole , during which heart fills. Heart is primarily an elastic organ. Whenever the filling is is more ventricle is stretched more ( diastolic filling is the stretch ) and the subsequent force of contraction is more . This is the basis of famous frank starling law.
LV filling is dependent on RV filling which in turn depend on venous return ..Venous return is a function of vascular tone and the persons physical activity .
Apart from this adrenergic drive make the heart contract vigorously . This is the reason , many patients with severely compromised LV function in ICU , supported with inotropic agents show vigorous contraction of heart .(Basis of doubutamine stress test )
** Every one of us is aware about the huge influence the preload has , on LV contractility . Surprisingly, it can also swing with changing after load . This fact is often under recognised .This is called Anrep effect .
So , imagine the scenerio . . .the heart is simply a “squeezing- slave” of pre load and after load ! . . . And still we are happy with assessing the cardiac function , in isolation without giving any respect to the loading conditions.
Final message
EF , would rank first among all medical investigations , that is significantly flawed , still continue to enjoy huge popularity ! It has little value as a screening test for assessing LV function in general population . But , it has an important role to assess the damage following MI and in the follow up of patients with significantly compromised LV function.
Cardiologist are aware of this fact , but most non cardiologists , especially Anesthetists and Surgeons revere the EF% with sanctity . This is definitely un-called for . It is the duty of the cardiologists to pass on this message to their colleagues in other fields.
Read Full Post »